"Trapped" nerves can be very painful and limit your ability to move or use the affected limb. They are often problematic at night-time, wreaking havoc with your sleep. Pins and needles, numbness, a weak feeling, and sharp pain are often symptoms produced by "trapped" nerves. There are many common sites for nerves to become symptomatic; often this could be at the spine, or further along a nerve into your hand or foot.
If you think you have a trapped nerve, you should have it checked over as it is always important to assess the severity, to locate where the nerve is "trapped", and to establish the cause. Once you have all this information you can start the right course of treatment, which is often a combination of physical therapy and pharmacological intervention. We will write to your GP if we think it would benefit you to have a certain prescription.
*Nerves are very rarely truly "trapped". In reality there is often more than enough space for the nerve to function, however nerves can be sensitive, and so slight changes in their ability to move or in the space which they occupy can create tension along the nerve leading to symptoms. Other local tissue changes, such as inflammation from another injury, can also cause a nerve to become symptomatic.
There are multiple causes for nerves to become symptomatic or "trapped", this can happen to peripheral nerves all over the body. Read below for more information.
A trapped nerve, also known as a pinched nerve, occurs when excessive pressure is applied to a nerve by surrounding tissues such as bones, muscles, tendons, or cartilage. This pressure can cause various symptoms, which may vary depending on the location and severity of the nerve compression. Here are some common symptoms associated with a trapped nerve:
- Pain: Persistent or intermittent pain is a common symptom. The pain may be sharp, burning, or radiating along the path of the affected nerve. It can worsen with certain movements or positions.
- Numbness or tingling: You may experience sensations of numbness or tingling in the area supplied by the affected nerve. This sensation is often described as pins and needles or a "falling asleep" sensation.
- Weakness: Muscle weakness may occur in the affected area. You might have difficulty gripping objects, lifting things, or performing tasks that require fine motor skills.
- Radiating pain: If a nerve in the spine is affected, the pain may radiate along the nerve pathway and travel to other parts of the body. For example, a pinched nerve in the lower back can cause pain that radiates down the leg.
- Muscle spasms: In some cases, muscle spasms may occur around the compressed nerve. These spasms can be painful and lead to further irritation of the nerve.
Sensitivity to touch: The area around the trapped nerve may become sensitive to touch or pressure. Even light touch or gentle pressure can cause pain or discomfort.
Yes, poor posture can contribute to the development of trapped nerves. When you maintain an incorrect posture for extended periods, it can put excessive pressure on certain nerves, leading to compression or irritation.
Here's how poor posture can contribute to trapped nerves:
- Forward Head Posture: When you consistently slouch or position your head in a forward position, it places strain on the nerves in the neck and upper back. This can lead to conditions like cervical radiculopathy, where the nerves exiting the cervical spine become compressed or irritated.
- Rounded Shoulders: Slouching or having rounded shoulders can cause compression of the nerves that pass through the shoulder region. This can result in conditions such as thoracic outlet syndrome, where nerves (brachial plexus) and blood vessels are compressed between the collarbone and the first rib.
- Prolonged Sitting: Sitting for long periods without proper posture can contribute to nerve compression, especially in the lower back and buttocks. It can lead to pain, numbness, and tingling that radiates down the leg.
Yes, stress can trigger or exacerbate nerve pain. While stress itself does not directly cause nerve pain, it can contribute to the worsening of existing nerve conditions or increase sensitivity to pain. Here's how stress can affect nerve pain:
- Increased Muscle Tension: Stress often leads to increased muscle tension and tightness. When muscles are tense, they can compress or irritate nearby nerves, resulting in pain or exacerbation of existing nerve pain.
- Heightened Sensitivity: Stress can lower the pain threshold, making individuals more sensitive to pain. This heightened sensitivity can cause nerve pain to feel more intense or be perceived as more bothersome than usual.
- Inflammation: Chronic stress can lead to inflammation in the body. Inflammatory processes can irritate nerves, amplifying pain signals and contributing to nerve pain symptoms.
- Altered Pain Processing: Stress can affect the way pain signals are processed in the brain. It can lead to changes in neurotransmitter levels and the perception of pain, potentially intensifying nerve pain.
- Impaired Immune Function: Prolonged stress can weaken the immune system, making it less effective at managing inflammation and promoting healing. This can prolong nerve pain and delay recovery.
It's important to note that stress-related nerve pain can be complex, and individual responses may vary. Managing stress through various techniques, such as relaxation exercises, mindfulness, stress-reducing activities, and seeking support from mental health professionals, can help alleviate stress-related nerve pain. Additionally, it's essential to address the underlying nerve condition with appropriate medical treatment and consult with a healthcare professional for guidance on managing both the nerve pain and stress levels effectively.
Yes, muscles can put pressure on nerves, leading to compression or irritation. When muscles become tense, or tight they can impinge on nearby nerves, causing pain and other symptoms. This compression can occur at various points along the pathway of the nerve, including where it exits the spine, passes through narrow anatomical spaces, or runs between muscles and other tissues. Here are some examples:
- Muscle Spasms: Sudden, involuntary muscle contractions or spasms can exert pressure on surrounding nerves, resulting in nerve compression and pain.
- Muscle Imbalances: Imbalances in muscle strength or tightness can lead to abnormal movement patterns and postural deviations. This can cause certain muscles to become overactive or hypertonic, potentially compressing nerves that run through or near those muscles.
- Trigger Points: Trigger points are tight knots or bands of muscle fibers that form due to muscle tension or overuse. These points can refer pain to other areas and may mimic a trapped nerve, however trigger points are muscular in origin and are relatively simple to treat.
It's important to address muscle-related issues to alleviate nerve compression. This can involve various approaches, including stretching exercises, strengthening weak muscles, correcting postural imbalances, using heat or cold therapy, physical therapy, and employing techniques to reduce muscle tension and stress.
Yes, sleeping in a funny position can potentially trap a nerve and lead to symptoms of nerve compression or irritation. When you sleep in an awkward or unusual position, especially for an extended period, it can put pressure on certain nerves, causing temporary compression or irritation. This can result in symptoms such as pain, numbness, tingling, or weakness.
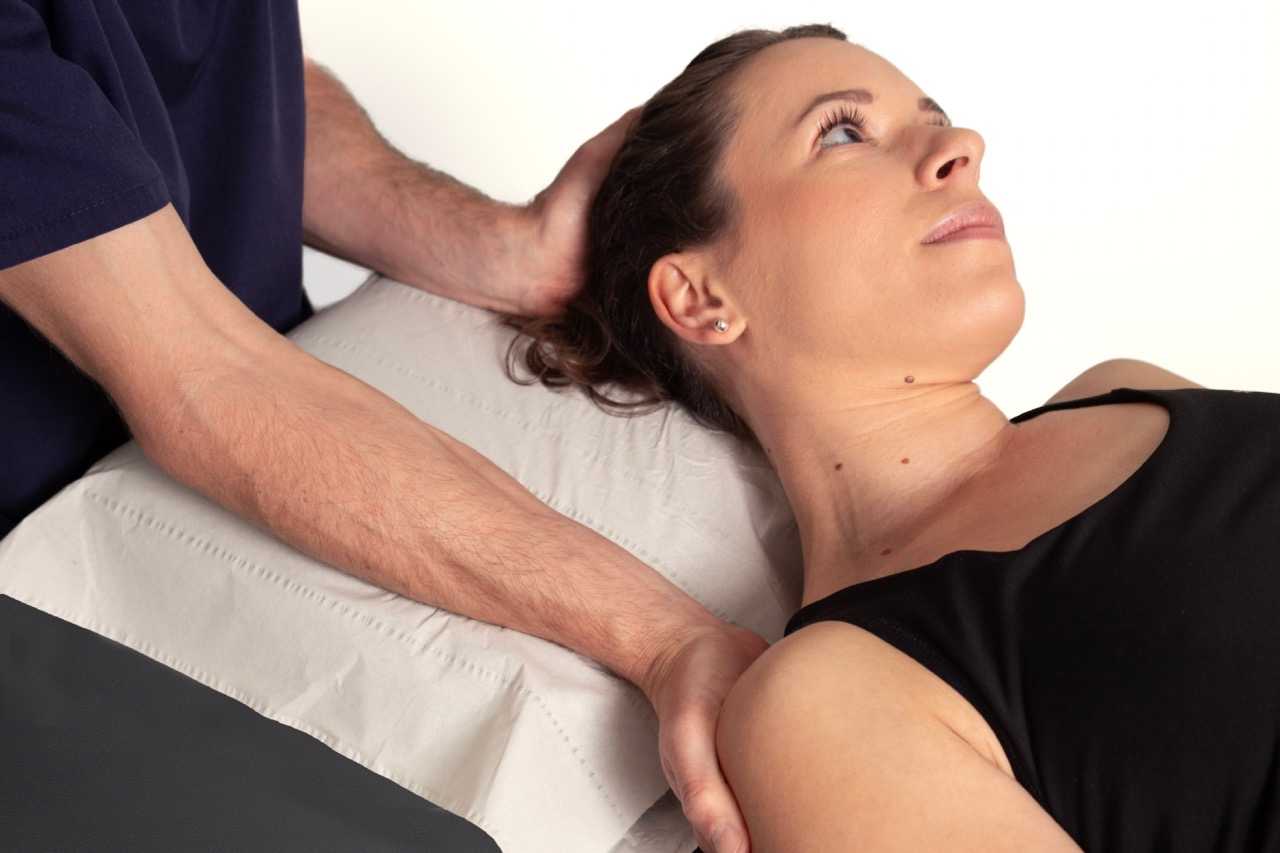
Massage and manipulation can be beneficial for trapped nerves in certain cases. These techniques can help alleviate muscle tension, reduce inflammation, improve blood circulation, and promote relaxation, which can indirectly relieve the pressure on the affected nerve. Here's how massage and manipulation can be helpful:
- Muscle Relaxation: Massage techniques, such as deep tissue massage or trigger point therapy, can help relax tight muscles surrounding the trapped nerve.
- Improved Blood Flow: Massage can increase blood circulation to the affected area, which can facilitate the delivery of oxygen and nutrients to the tissues. Improved blood flow can support the healing process and reduce inflammation, potentially easing nerve compression symptoms.
- Pain Relief: Massage stimulates the release of endorphins, which are natural pain-relieving chemicals in the body. By reducing pain perception, massage can provide temporary relief from nerve pain symptoms.
- Improved Range of Motion: Manipulation techniques from an Osteopath or Physiotherapist, can help restore proper alignment and mobility of the spine or joints. This can alleviate nerve compression caused by misalignments or joint restrictions, leading to symptom improvement.
However, it's important to note that not all cases of trapped nerves can be effectively treated with massage and manipulation. The underlying cause and severity of the nerve compression should be taken into consideration. In some cases, certain manipulative techniques may not be suitable or may even exacerbate the condition. An Osteopath or a Physiotherapist will be able to assess the severity and underlying cause of the trapped nerve and determine if massage and manipulation are appropriate as part of a comprehensive treatment plan advise on the most appropriate treatment for you.
The choice of medication for nerve entrapment syndromes depends on several factors, including the severity of symptoms, the underlying cause of the nerve entrapment, and individual patient characteristics. Over the counter medications are generally safe to try, unless you are taking other medications which interact with them. If your symptoms are particularly severe it may be worth speaking with your GP, as they can prescribe other types of medication which can help.
It's important to note that medication alone may not address the underlying cause of nerve entrapment. Therefore, a comprehensive treatment approach may involve a combination of medication, physical therapy, lifestyle modifications, and other interventions tailored to the specific condition and needs of the individual. An Osteopath or Physio will be able to advise what is best for you.
The approach to rest or movement with nerve pain will vary depending on each individual. In general, it's best to strike a balance between rest and movement, taking into account the severity of the pain and individual circumstances. Here are some considerations:
- Rest: Resting during acute flare-ups of nerve pain can be beneficial to allow the affected nerve to calm down. Short periods of rest can help alleviate pain and prevent further aggravation. However, prolonged or excessive rest may lead to muscle stiffness, weakness, and potential deconditioning, which can hinder recovery in the long run.
- Gentle Movement: While rest is important, gentle movement and activity are often encouraged for nerve pain management. Movement helps improve blood circulation, maintain muscle strength and flexibility, and prevent muscle imbalances. Gentle exercises, such as stretching or low-impact activities, can help reduce muscle tension and promote healing.
- Avoid Aggravating Movements: It's essential to avoid activities or movements that worsen nerve pain or exacerbate symptoms. These may include repetitive motions, heavy lifting, or positions that directly compress or irritate the affected nerve. Identify and modify any activities that contribute to pain or discomfort.
- Gradual Progression: If movement is well-tolerated and does not significantly increase pain, gradually increasing activity levels can be beneficial. Start with gentle exercises and gradually progress to more challenging activities as pain allows. It's important to listen to your body and not push through severe pain or worsening symptoms.
- Professional Guidance: Consult with a healthcare professional such as a Physio or Osteo who can provide specific guidance and recommendations based on your condition. They can develop an individualized exercise program, provide techniques for pain management, and monitor your progress.
Heat or cold compresses can be beneficial for trapped nerves as it helps promote relaxation, improve blood circulation, and reduce muscle tension, which can indirectly alleviate the pressure on the affected nerve. Hot and cold therapy aims to increase muscle relaxation and blood circulation to the effected area.
There are some instances when applying heat or raising your body temperature may actually aggravate your nerve symptoms, should this happen, simply remove the heat and rest until your body has gradually cooled. Report this symptom to your clinician and they will be able to provide you with other tactics to help your symptoms.
Relax..... Pretty hard to do when the pain is really gripping! There is no instant cure with nerve pain unfortunately, however a combination of the following tactics will gradually reduce your symptoms until you are back to your normal self!
- Rest: Allow the affected area to rest and avoid activities or positions that exacerbate the nerve compression. Take breaks from repetitive or strenuous activities that may contribute to the symptoms.
- Gentle Stretching: Perform gentle stretching exercises that target the muscles surrounding the trapped nerve. Consult with a healthcare professional, to learn specific stretches that can help relieve nerve compression and improve flexibility.
- Heat Therapy: Apply heat to the affected area using warm compresses, heating pads, or warm baths.
- Cold Therapy: Cold therapy, such as applying ice packs or cold compresses, may help reduce inflammation and numbness associated with nerve compression.
- Pain Medication: Over-the-counter pain relievers, or medication a GP can prescribe.
- Good Posture: Maintain proper posture and body alignment to prevent unnecessary strain on nerves and muscles.
- Stress Reduction: Practice stress-reducing techniques such as deep breathing exercises, meditation, or mindfulness. Chronic stress can contribute to muscle tension and worsen nerve compression symptoms, so managing stress levels can help relax the body and relieve the trapped nerve.
- Physical Therapy: Consider seeking the guidance of a physical therapist who can provide manual therapy techniques, and advice on the cause of the nerve pain.
It really depends on the cause as to the recovery time for your nerve entrapment. Simple causes such as muscle tightness can be relieved within a couple of weeks of stretching, other causes can take 6-12 months to heal. It is important to seek a diagnosis for your nerve entrapment so you can receive appropriate treatment.
The curability of nerve entrapment depends on several factors, including the underlying cause, the severity of the condition, and the specific nerves involved. In many cases, nerve entrapment can be effectively managed and symptoms can be significantly reduced or eliminated with appropriate treatment. However, complete resolution of symptoms may not always be achievable, especially in chronic cases.
Early diagnosis, timely intervention, and adherence to treatment recommendations can increase the likelihood of successful outcomes. It's important to work with a healthcare professional who can accurately diagnose the underlying cause of the nerve entrapment and guide you through an appropriate treatment plan.
This depends on the severity of your symptoms, if they are severely disturbing your quality of life then it is always worth speaking with a GP. However, it can be worth seeing an Osteopath or a Physiotherapist first who will better able to diagnose and confirm a nerve entrapment syndrome. You can then take this information to the GP which will help them provide the best type of medication for you.
In most cases, a diagnosis of nerve entrapment or trapped nerve can be made based on a thorough medical history, and physical examination.
Imaging studies, such as MRI, are not always necessary for diagnosing nerve entrapment. However, there are situations where an MRI may be ordered to provide more detailed information or to rule out other possible causes of your symptoms. An experienced clinician will be able to give guidance on the need for imaging.



